Going ‘low FODMAP’ has boomed in popularity in recent years, yet there’s so much confusion around the diet. And going at it alone can be risky business without a clear action plan.
In a nutshell: The low FODMAP diet can be effective for helping with IBS symptoms, but it’s NOT a panacea or a long-term solution and it’s super important to reintroduce them gradually – your gut microbes will thank you!
First, what exactly are FODMAPs?
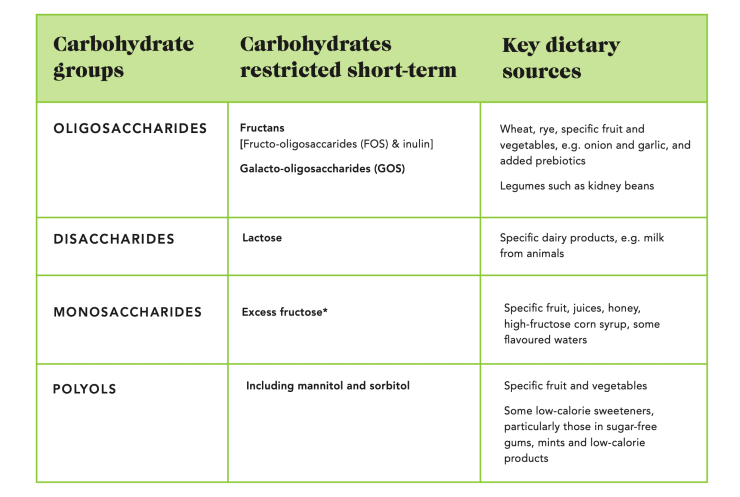
FODMAP stands for fermentable, oligosaccharides, disaccharides, monosaccharides and polyols – and these are types of carbohydrates that aren’t completely absorbed in the small intestine (where most of our food is usually absorbed). Instead, they travel down into the large intestine, where they draw excess water in and add pressure on the intestinal wall. Here, our gut microbes feast (or “ferment”) them too, which can trigger some gut symptoms (like bloating, gas and stomach pain) in some people with IBS. This is a totally natural process and they’re by no means inherently ‘bad’ – they’re present in a lot of our plant-based foods and many FODMAPs are prebiotics (food that feeds your gut microbes). But if you have a sensitive gut and prone to IBS symptoms, you’re likely to feel the effects on the gut more.
Taken from Eat Yourself Healthy & Love Your Gut
What’s the evidence for reducing FODMAPs for IBS?
Unlike the many fad diets out there, the low FODMAP diet has been carefully and specifically developed for people with irritable bowel syndrome (IBS) and importantly it’s backed up by clinical research – as such, it’s considered a medical diet. Dietary strategies have transformed how we can manage IBS, which makes sense as 9 in 10 people with IBS say food triggers their symptoms. If you have IBS, studies show there’s a 70% chance your symptoms will improve with a low FODMAP diet in the short term. But that doesn’t mean those magic claims about cutting out perfectly healthy foods to beat gut issues are valid – there are so many myths about the low FODMAP diet out there, but it’s certainly no panacea for IBS or a cure-all.
Before you even consider trying a low FODMAP diet…
- Is it definitely IBS? If you’re getting gut symptoms and think it might be IBS, it’s super important to check with your GP or physician to rule out any other underlying issues (e.g. coeliac disease) – so don’t be in a hurry to assume it’s IBS.
- If it is IBS, have you tried any techniques to manage your stress levels? These target the underlying cause: the gut-brain axis (the two-way communication between the gut and brain). (There are more mindfulness exercises in my book too)
- If you have a history of disordered eating, it’s really important to see a dietitian for support to get the best care for you personally. Restricting foods can trigger a relapse.
- It’s not just what you eat but how you eat that can have an impact. Try the first-line approaches that’s been shown to have impressive benefits for around 50% of IBS sufferers. This involves limiting spicy food, high-fat fast foods, alcohol and caffeine, alongside spreading fibre intake across the day, going for whole fruits instead of juices or smoothies (1 per sitting) and staying hydrated.
I’ve been recommended to try the low FODMAP diet by my GP/physician – how does it work?
The low FODMAP diet essentially consists of 3 stages: Restrict, Reintroduce, Personalise. But it’s not an easy diet to follow without the help of a trained dietitian and there isn’t a one-size-fits-all, everyone’s IBS is different!
- Restricting all high-FODMAP foods to give your sensitive gut some down time for 4-8 weeks. It’s really important to make sure you’re still filling your nutrient needs, so try to keep up your plant-based diversity across all the lower FODMAP foods. I’d recommend doing this stage alongside 15 minutes a day of mindfulness exercises and/or yoga. If you haven’t had any relief after 6 weeks, go back to your usual diet and explore other strategies (with a specialist dietitian if you can, we’re always here to help at The Gut Health Clinic).
- Reintroducing each of the different FODMAPs one by one. The portions are best to be guided by a dietitian – as a general guide I recommend starting with around ⅓ of your normal portion and slowly building up from there.
- Personalising your diet for the long-term, based on your tolerance level to FODMAP foods. This is essential to give you more flexibility and a more varied diet – not to mention your quality of life (and social life). The good news is that tolerance tends to improve over time, as you continue with those stress-management techniques targeting the gut-brain axis. Even if you find you don’t tolerate certain foods at first, that’s why it’s a good idea to re-test overtime – diversity is still the aim of the game.
6 things you need to know
- Those FODMAP food lists online usually aren’t accurate or complete, so stay away from Dr Google and see a FODMAP trained dietitian instead. If you don’t have access to a FODMAP-trained dietitian or are on the waiting list to see one, you may like to try my ‘FODMAP-lite’ approach which is a much less risky approach to do on your own. See my book for a step-by-step guide.
- It’s not FODMAP-free. Foods are split into ‘low’ or ‘high’ FODMAPs per portion, so the low-FODMAP foods can still contain some.
- Portion sizes are key. Reducing the portion size can make a high-FODMAP food low-FODMAP. For example, one cup of cooked wheat pasta is high-FODMAP, but if you just have ½ a cup, that’s low.
- FODMAPs are carbs. So it’s safe to say almost zero-carb foods such as eggs, fish and oils are FODMAP-free.
- It’s not gluten-free. Yes it does restrict gluten-containing grains (wheat, barley, rye) but that’s because of the fructans (which is a FODMAP), not the gluten.
- You can still have lactose if you’re confident you’re not lactose intolerant (and even then, you can still enjoy small amounts of up to 50ml per sitting).
- Keep up your fibre and calcium intake by enjoying plenty of low FODMAP fibre foods, such as raspberries, strawberries, green beans, spinach, quinoa, oats and flaxseeds; as well as sources of calcium including hard and aged cheese, canned fish with edible bones, calcium-fortified plant-based milks.
Why is reintroduction so important?
It’s not meant to be an ‘avoid for good’ diet – it’s also a way to test your tolerance to different FODMAP foods so you can personalise your diet long-term. FODMAP foods nourish your gut microbes and it’s so important not to banish them for good – the diet can starve your gut bacteria, and we definitely don’t want them to go hungry. That’s why the initial restriction phase should only be done for a maximum of 8 weeks. Reintroduction is essential for the best long-term health outcomes and to make sure you’re getting all the nutrients your body needs – as well as for you to enjoy all the amazing flavours of plant-based diversity again!
Still fearing FODMAPs?
I know many of you with sensitive guts and IBS may be a little reluctant to reintroduce foods back into your diet – but in my 11 years of being a dietitian, I’m yet to meet a gut that can’t reintroduce them, and I’ve met thousands! It really is possible for everyone to include these gut-loving FODMAP foods in their diet. The key is to go slowly, at your own pace, to find your own tolerance level that works for you.