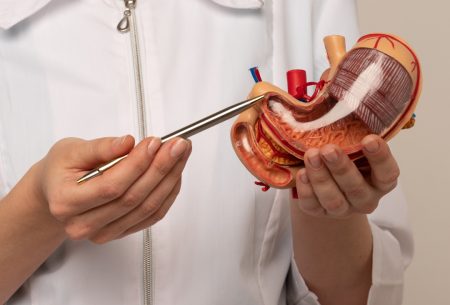
Let’s start by considering what the pancreas is, and what it does
The pancreas is an important gland in your digestive system that has 2 main functions. It releases digestive enzymes into your small intestine when you eat, which help you to digest your food and absorb the nutrients from it. It also releases the hormones insulin and glucagon which help your body regulate blood sugar levels.
What is pancreatitis?
Pancreatitis is essentially where the pancreas becomes inflamed (swollen), and this can be either acute (short-term) and chronic (long-term).
There are many causes of pancreatitis including autoimmune conditions, infections, post-operative issues, trauma, medications, genetics, and cystic fibrosis in children. But the most common causes we see are:
- gallstones
- drinking too much alcohol
Some symptoms are similar for both acute and chronic pancreatitis:
- severe and sudden tummy pain, which can radiate to your back
- nausea and vomiting
- diarrhoea
- indigestion
- yellowing of the skin (aka jaundice)
- fever
- increased heart rate
Acute pancreatitis
This is the sudden inflammation of the pancreas, and in most cases people start to feel better within about a week and have no long-term problems. However, it can range from mild to severe or life-threatening with serious complications requiring prolonged hospital admissions.
Treatment for acute pancreatitis aims to help control the condition and manage any symptoms. Eating and drinking can become difficult and make individuals feel worse, and so a hospital dietitian is usually involved to support someone’s nutritional status whilst managing and minimising complications. The dietary management may include some complete gut rest for a few days as trying to digest solid food could put more stress on an already inflamed pancreas. Sometimes a liquid or modified diets is prescribed by your dietitian and medical team, and in some cases individuals may require artificial nutrition support which may be in the form of liquid formula nutrition delivered directly into your gut via a tube (aka enteral nutrition) or “parenteral nutrition” which is prescribed nutrition delivered directly into veins to provide the body with nourishment whilst bypassing the gut completely.
Chronic pancreatitis
This is a long-standing inflammation which develops over longer periods of time where the pancreas becomes permanently damaged and stops working as well as it should, and alongside the symptoms mentioned earlier, you may also experience weight loss and symptoms of diabetes such as excessive thirst, frequent urination and feeling very tired.
Whilst the damage is permanent, there’s no cure for chronic pancreatitis, treatment can help manage symptoms and improve quality of life. This can include pain management and occasionally surgery or non-surgical procedures. Often digestive enzyme supplements are prescribed to enable your body to break down food and absorb nutrients properly where the pancreas may no longer be able to do this sufficiently on its own, which is what can lead to weight loss and nutritional deficiencies. Note that these prescription enzymes are much higher doses than you can buy yourselves online (which we don’t tend to recommend to people anyway), and should always be managed by a specialist dietitian and your GP. We’ll be doing a post about Pancreatic Enzyme Replacement Therapy (PERT) in a few weeks for pancreatic cancer awareness month.
One of the signs that you may need to have PERT is if your poop becomes paler, greasy, very smelly, loose and difficult to flush. So if you notice these symptoms please discuss it with your GP as they may want to do a stool test to check for pancreatic enzyme insufficiency.
Prevention of pancreatitis
As gallstones or excessive alcohol are the predominant causes, a healthy diet and lifestyle can help reduce your risk of developing pancreatitis or prevent a recurrence of acute pancreatitis.
Quick tips:
- Maintaining a healthy body weight (regular exercise can help)
- Limit foods with a high saturated fat content (cakes, biscuits, pastries, processed meats)
- Consume more wholegrains – aim for three serves of wholegrain cereals per day (bread, pasta, oatmeal, brown rice to name a few).
- Aim for a varied and plant-based diet (yep, go for that 30+ plants per week!)
- Limit alcohol consumption
Summary
Though it’s relatively small in comparison to our other digestive organs, the pancreas has key roles in our digestion and metabolism, meaning pancreatitis can lead to a wide range of nutritional issues. We recommend seeing an experienced dietitian who can support you with a personalised nutritional plan if you have damage to your pancreas. Your GP or gastroenterologist can refer you for this. Alternatively we have experts on our team who specialise in this so please contact us via the website to arrange an assessment.
This blog was authored by Tanzil Miah, an IBD and surgical specialist dietitian.