Test your intolerance – take the 3-step lactose challenge
So you suspect you have lactose intolerance because every time you enjoy a latte, creamy pasta or ice cream, your gut tells you it isn’t happy. If you’re struggling with waiting lists or would rather play food detective at home, put down Dr Google and take this lactose challenge to help determine whether lactose really is the culprit. Aim to do this blinded, which, in research speak, means that you are unaware if you are having the lactose-containing product or a placebo (i.e., a matched food that doesn’t contain lactose). This comes back to the gut:brain axis. Remember: the communication between the two is bidirectional, which explains why if we perceive something to be bad for us (even if it’s not), it can actually manifest in physical gut symptoms. Blinding a food challenge removes this type of bias.
Step 1. 48 hours prior to each challenge
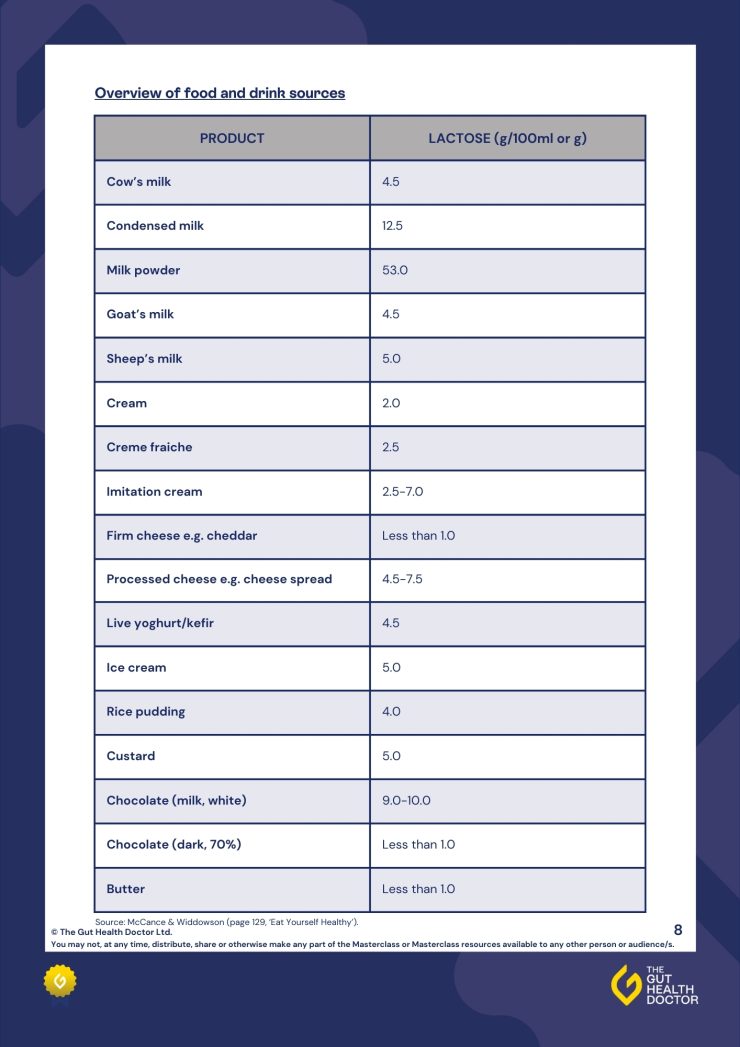
Swap all lactose-containing foods for low lactose foods**. Following a low lactose diet for 48 hours prior to and during the challenge will ensure your trial is more accurate.
Step 2. To prepare, you will need:
- 400mls of low fat cow’s milk (active challenge).
- 400mls of low fat lactose-free cow’s milk (placebo challenge).
- A loved one or friend. They will be in charge of blinding you to the different challenges. Ask them to disguise the milk so you can’t tell the difference between the active and the placebo.
Step 3. Begin the challenge:
- Test your milks one week apart, on the same day and ideally at the same time. So, if you choose a Wednesday evening for the first challenge, stick to the following Wednesday evening for the second challenge. This will help keep the testing conditions the same.
- Remember to continue on a low lactose diet during and for 24 hours following the challenge.
**Check out this comprehensive lactose resource for more tips on completing this lactose challenge (including a detailed list of what foods contain lactose) and managing your intolerance.









 What’s the difference between an allergy and an intolerance?
What’s the difference between an allergy and an intolerance?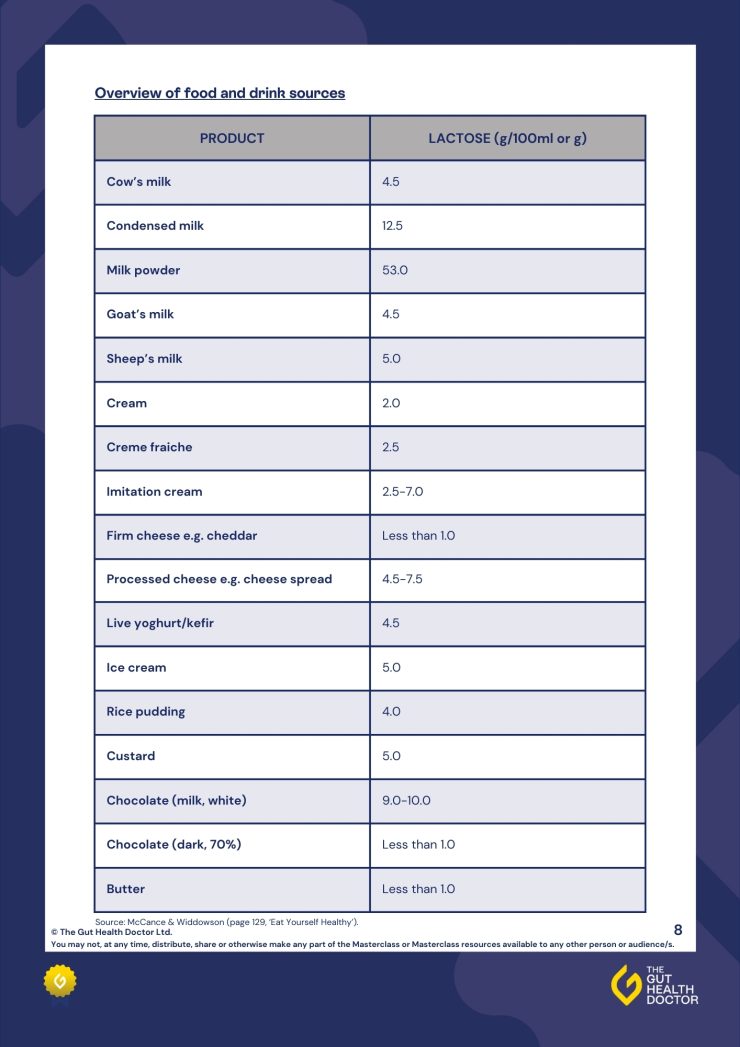
 1. Go slow and steady
1. Go slow and steady  2. Make a meal of it
2. Make a meal of it 3. Get funky with fermented foods
3. Get funky with fermented foods 4. Supps up
4. Supps up Say Cheese
Say Cheese