Firstly, let me start by saying antibiotics are incredibly important. They’re powerful, life-saving medications and it’s thanks to antibiotics that serious, potentially fatal, infections can be cured. But there’s been a growing issue: the overuse of antibiotics. And, as with most things, overdoing it could have some unwanted side effects.
That doesn’t mean antibiotics are ‘bad’ – far from it. However, it does mean it’s worth sparing a thought for how they can impact your gut, and overall, health in the long run. So, with the intention of empowering you with knowledge (without any of the guilt or scare-mongering!), let’s dive into what effect antibiotics can have on our gut microbes – and my top tips for when you do need to take them.
What actually are antibiotics?
An antibiotic is essentially a type of antimicrobial substance designed to target bacteria, either preventing the growth or killing the bacteria (‘antibiotic’ literally translates to ‘anti-life’ in Greek).
Some antibiotics are specialised to target certain specific ‘bad’ bacteria, while others can target a wider group (aka broad-spectrum antibiotics) – including the beneficial types.
How do they affect our gut microbes?
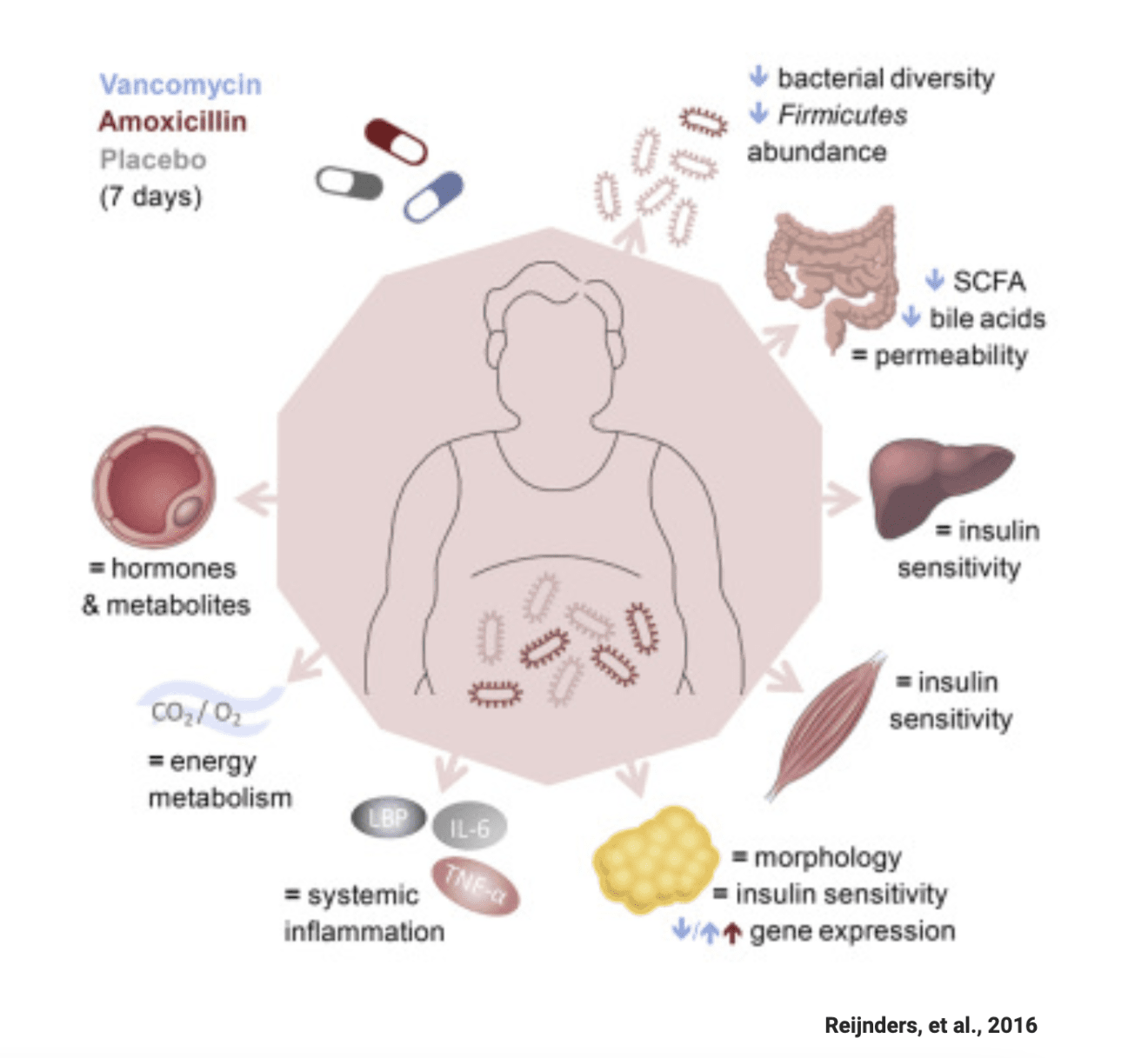
By targeting bacteria, antibiotics can disrupt your gut microbiota (GM), which can lead to diarrhoea – known as antibiotic-associated diarrhoea. It’s estimated that 30% of people experience loose poops when taking antibiotics.
Depending on the type and dose of antibiotics, a 2020 review suggested that in most cases our gut microbiota returns to (near) normal within a few weeks. However, a 2015 study showed it can take up to 12 months for our GM to “bounce back” after antibiotics, and in some people, even at 12months their GM still hadn’t fully recovered. This is why it’s worth being cautious and making an informed decision before taking them.
What does ‘antibiotic resistance’ mean?
Antibiotic resistance can happen when bacteria adapt to become ‘resistant’ to antibiotics that were designed to destroy them, due to changes in the DNA of the bacteria.
They’re able to grow and create infection, even when faced with antibiotics.
The result? Certain antibiotics will no longer be effective in treating certain infections, meaning the treatment for these infections becomes much more difficult.
The more frequently antibiotics are used, the more likely they are to become ineffective for treating more serious conditions – which could be dangerous, or even life-threatening.
Ultimately, antibiotic resistance highlights just how smart our microbes are – they can change and adapt quickly, as we’ve also seen with new strains of COVID-19.
What’s being done about it?
It’s no longer common practice in healthcare to use antibiotics for treating chest infections, ear infections or sore throats. Global health organisations are working to limit antibiotic use, particularly for mild health issues that can heal on their own.
What you can do
Next time your GP or physician advises that antibiotics aren’t necessary for you, it’s worth taking it seriously. My husband (who is an NHS GP in the UK) is often pushed by patients for antibiotics for common colds – but as they’re viral (i.e. caused by a virus) not bacterial, antibiotics that only target bacteria don’t work.
That said, sometimes taking antibiotics is unavoidable, so here are three things worth doing.
Top tips if you need to take antibiotics
1. Eat plenty of prebiotic foods that help good bacteria thrive via a diverse range of fibre-filled foods – hitting your 30 plant points a week across fruits, vegetables, wholegrains, legumes, nuts and seeds.
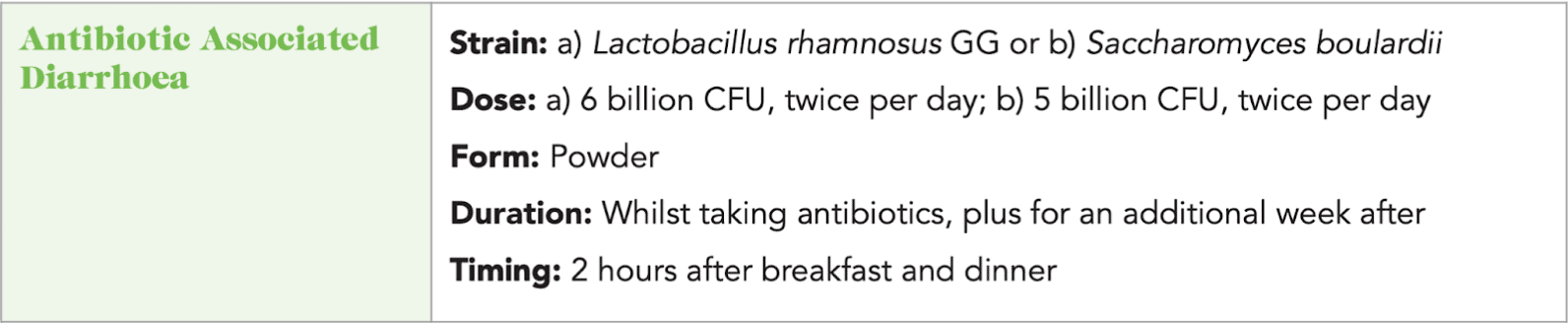
2. Consider a probiotic. Taking a specific probiotic while you’re taking antibiotics, and continuing for a week after, has been shown to significantly decrease your risk of antibiotic-associated diarrhoea. Check out my Probiotic Prescriptions here. There is NO convincing evidence that you should take a probiotic after you have finished your antibiotics, indeed one small study suggested this may even slow down the recovery of your GM.
3. Complete your course. Make sure to finish your full course of antibiotics, even if you feel better (this can help prevent antibiotic resistance).